- Research
- Open access
- Published:
Social-emotional and behavioural problems in young children of healthcare worker mothers during the COVID-19 outbreak: a case-control study
BMC Psychiatry volume 24, Article number: 407 (2024)
Abstract
Background
The pandemic has had a significant impact on the daily lives of children and their families, particularly the children of health care workers, due to changes in family routines as a result of their parents’ work schedules. We aimed to explore the socioemotional and behavioural (SEB) problems of children of healthcare worker mothers (HCWM) during the COVID-19 pandemic and compare them with age-matched children and their mothers from other occupations.
Method
A case-control study design was applied, and a snowball approach was used to enrol volunteered participants aged between 6 and 36 months of age, through a Google survey. We used the Brief Infant-Toddler Social and Emotional Assessment (BITSEA) questionnaire to assess children’s SEB problems and a Brief Symptom Inventory (BSI) to evaluate the psychological distress of mothers. Differences in BITSEA, BSI and MSPSS scores were examined using chi-square and Mann-Whitney U tests, as appropriate. A logistic regression model was used to identify independent predictors of children’s behavioural and emotional problems.
Results
In total, 600 questionnaires were analysed. It was observed that children in the HCWM group were separated from their mothers more often and for longer periods of time than their counterparts (p < 0.010, p = 0.002). Changes in the child’s structured outdoor activities during the pandemic period were more likely to be observed in the HCWM group (p < 0.05). The percentage of children with the BITSEA problem subscale above the subclinical cut-off, externalizing and dysregulation scores were significantly higher in the HCWM group (p = 0.044, p = 0.031, and p = 0.016). Moreover, each point increase in BSI global index scores (p < 0.001, RR:3.34, 95%CI:1.91–5.82) was found as a risk factor for clinically significant SEB problems.
Conclusion
Overall, the current study suggests HCWM’s have experienced occupational inequality, and young children of HCWM’s were at increased risk for externalizing and dysregulation problems during the pandemic. Maternal psychological stress had a significant impact on their children’s socio-emotional well-being.
Introduction
The COVID-19 epidemic began in China, spread quickly to other countries, and has been declared a public health emergency of international concern on January 30th 2020 by the World Health Organization (WHO) [1]. Figures from around the world show that approximately 7 to 11% of healthcare workers (HCWs) have been diagnosed with COVID-19 [2]. Political measures adopted to control the disease such as closure of childcare services, and disrupted socialization exacerbated existing inequities and posed additional challenges for HCW mothers (HCWM) with young children [3]. They had to balance work responsibilities such as providing patient care against their responsibilities to protect their own well-being from the effects of chronic stress and their children’s mental health [4]. HCWMs with young children raised their concerns about access to childcare, parenting, and household duties [5]. Inability to find caregivers and elderly parents for childcare support was a significant contributor to this inequity. While there is limited research on this specific topic, these challenges may have contributed to increased child behaviour problems particularly at a young age. In addition, as noted in the United Nations report on Turkey’s gender equality performance from 2000 to 2019, Türkiye still maintains a strong traditional division of labour. Although it is improving day by day, women still spend four times more time than men on unpaid domestic work (the double burden of housework and childcare), which is not sufficiently shared by family members, especially men, increasing women’s workload [6].
Children of HCWMs were disadvantaged relative to their peers due to deprivation of maternal care for an extended duration, the risk of their parents contracting the virus, the fear of losing their parents, and changes in family routines due to their parents’ work schedules [7]. Trauma faced at a young age may have long-term adverse developmental consequences across their lifespan [8].
Studies have shown that HCWs have experienced higher levels of stress, anxiety, and depression compared to the general population during the pandemic [9,10,11]. Notably, parental distress can be a significant contributor to child behavioural problems. Distressed parents tend to demonstrate emotional unavailability thus leading to the occurrence of child behaviour problems [9, 12]. On the other hand, parental distress has been shown to be associated with lack of social support. It has been shown that social support provided by family and friends can help reduce parental distress and have a positive effect on parenting behaviours. Due to social distancing measures these protective close relationships of families were cut off [10]. Social support plays an important role in a person’s mental health, and even more in disasters acts as a buffer against the negative effects of trauma-related events, minimizing the potential of developing negative consequences [11, 13]. Therefore, measuring the social support of HCWs would be of critical importance in planning interventions for this vulnerable population [7].
Overall, the pandemic has had a significant impact on the daily lives of children such as changes in daily routines, increased stress and anxiety, reduced physical activity, reduced peer interactions, increased screen time and changes in sleep environment which can contribute to sleep disturbances in young children [12, 14]. On the other hand, other studies have found that improved parent-child interactions due to home confinement could allow for better sleep [12, 14,15,16].
The study was planned based on the hypothesis that children of HCWMs experienced more socioemotional and behavioural (SEB) problems than children of mothers from other occupations during the COVID-19 pandemic. We aimed to explore SEB problems and sleep patterns in children of HCWMs; assess the psychological distress of mothers and their perceived social support during the COVID-19 pandemic, and compare them with age-matched peers and their mothers from other occupations.
Materials and methods
A case-control study was applied and a snowball approach was used to enrol volunteered participants. All women having children aged between 6 and 36 months of age were invited to participate via websites, social media and e-mail between August 18th 2020 - October 17th 2020. All surveys were conducted in Türkiye. Personal identifying information was not collected or recorded.
An online survey was developed on the Google platform securing data collection by a confidential login system which can be filled out through smartphones, tablets or computers. The questionnaire took approximately 15 min to complete. It was pilot tested on 15 mothers and found acceptable. Due to pandemic restrictions, the study has been promoted via social media (such as Whatsapp, Telegram doctor and parent groups, Instagram, websites) and they are being asked to send links to volunteers in their area. Volunteers were sent an invitation email or message with a link to an anonymous online questionnaire, depending on their contact preferences. To access the questionnaire, respondents were asked to read the informed consent form and tick the mandatory box. Questionnaire responses were converted to excel spreadsheets.
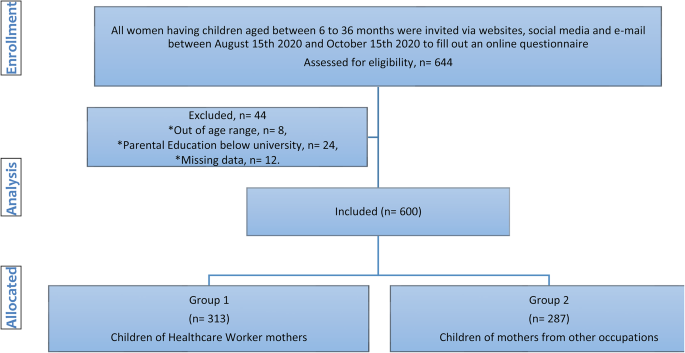
Children aged 6–36 months and working mothers aged 20–45 years with at least some college/university education were eligible to participate in the study. Children whose parents didn’t approve the consent form or who had a known chronic health problem were excluded from the study. Children of HCWMs were grouped as Group 1 (HCWM group), and children of mothers from other occupations were grouped as Group 2 (non-HCWM group). Doctors, nurses, and paramedics are considered as HCWMs. For two groups, the difference between the groups was predicted to be statistically significant at the medium effect size (according to the percentage of SEB and sleep problems in that age group), and the total sample size was calculated as 600 for 95% power and 0.05 alpha significance level, taking into account dropouts and other possible problems (Fig. 1).
Brief Infant Sleep Questionnaire (BISQ) [17,18,19,20] and Brief Infant-Toddler Social and Emotional Assessment (BITSEA) questionnaires [21,22,23] were used to assess children’s sleep, and social-emotional development, respectively. Multidimensional Scale of Perceived Social Support (MSPSS) [24, 25], and Brief Symptom Inventory (BSI) [26, 27] questionnaires were used to evaluate maternal social support and psychological distress.
Questionnaires
The BISQ functions as a tool designed to assess the early childhood sleep environment, covering aspects such as parental practices, daytime and night-time routines, and sleep issues, relying on responses from parents [17]. Through validation, BISQ demonstrated significant correlations with sleep measures obtained from actigraphy and sleep diaries. The Turkish translation of BISQ has been deemed acceptable, comprehensible, and reliable for evaluating sleep-related factors in infants [18]. In this study, maternal perception of sleep problems was categorized based on the expanded BISQ version. A parent-reported sleep problem was defined as moderate or severe while no problem was designated for those with no problem or a very small problem, as indicated in previous studies [17, 19]. Parents were asked a single question to assess the pandemic’s impact on their children’s sleep. The question of whether there was a change in their children’s sleep during the pandemic period and if the answer is “yes”, what has changed was added to the beginning of the BISQ survey. If the child woke up > 3 times/night and woke up after sleep onset (WASO) for > 1 h or spent < 1 SD of the study population’s sleep duration (10 h), the child was considered a poor sleeper [17, 20].
The BITSEA is a tool for screening social, emotional and behavioural development in early childhood which consists of 42 items [21]. The BITSEA encompasses two scales: the Problem scale (BITSEAp) with 31 items and the Competence scale (BITSEAc) with 11 items. Each item utilizes a response format with three choices: “not true/rarely” (0), “sometimes true/sometimes” (1), and “very true/often (2).” Problematic behavior is addressed in the externalizing (6 items, e.g., impulsivity, defiance, peer aggression), internalizing (8 items, e.g., fearfulness, worry, anxiety, sadness), and dysregulation (8 items, e.g., sleep and eating problems, negative emotionality, sensory sensitivities) domains [22]. Higher total scores on BITSEAp indicate a greater level of behavioral and emotional problems, while lower total scores on BITSEAc indicate a lower level of competence. The Turkish version of BITSEA has demonstrated reliability, validity, and simplicity, making it an effective instrument for screening social, emotional, and behavioral problems in toddlers [23]. Identified cut-offs of BITSEAp in gender groups for subclinical scores were ≥ 18 for males, and ≥ 21 for females. It was ≥ 24 for clinical scores in both genders [21, 23].
The MSPSS is a concise self-administered tool comprising 12 items, divided into three subscales [24]. Respondents rate each item on a seven-point Likert scale, ranging from 1 (very strongly disagree) to 7 (very strongly agree). A higher score on the Likert scale indicates a greater perception of social support. The total score, ranging from 12 to 84, can be calculated by adding the items within each subscale and then dividing by 4. The instrument assesses the level of social support and identifies its sources from family, friends, or significant others. Elevated scores are indicative of higher levels of perceived social support. The Turkish adaptation of MSPSS has demonstrated reliability, validity, and ease of application, establishing it as an effective tool for screening perceived social support [25].
The BSI comprises a self-report symptom inventory with 53 items, encompassing nine symptom dimensions: Somatization, Obsession-Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism; along with three global distress indices: Global Severity Index, Positive Symptom Distress Index, and Positive Symptom Total [26]. This instrument facilitates the evaluation of psychological distress and psychiatric disorders. Respondents rate items on a five-point Likert scale, ranging from 0 (not at all) to 4 (extremely), indicating the degree of distress experienced in the past week. Scores are generated for nine primary symptom dimensions and three global distress indices. The Turkish adaptation of BSI has demonstrated reliability, validity, and simplicity, making it a valuable tool for assessing maternal psychological distress, including depression, anxiety, hostility, negative self-perception, somatization, and global distress indices [27].
Statistical analyses
IBM SPSS Statistics software (version 28.0, IBM Inc., United States) was employed for all analyses. Descriptive statistics, including mean and standard deviations (SD) for normally distributed continuous variables, and median and quartiles for non-normally distributed data, were presented. Normal distribution conformity was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests. Categorical variables were summarized using frequencies and percentages. Differences in family characteristics, sleep parameters, BITSEA, BSI, and MSPSS scores were examined using the chi-square and Mann-Whitney U test, as appropriate. Given the non-normal distribution of all parameters, Spearman’s Rho Correlation analysis test was utilized to calculate correlation coefficients and assess significance.
Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were reported. To compare study group data with nationally representative data, a one-sample T-test and chi-square test were applied for sleep parameters, and the chi-square test was used for SEB problem frequency. In multivariate analysis, factors identified in univariate analysis, without collinearity, were entered into logistic regression to determine independent predictors of children’s behavioral and emotional problems. The Hosmer–Lemeshow test assessed the goodness-of-fit of the model. A 5% type-I error level was set for determining statistical significance.
Results
In total, 600 questionnaires were analysed, 313 children were included in the HCWM group and 287 were included in the non-HCWM group (Fig. 1). There were no statistically significant differences in maternal and paternal occupation between the groups. Although the mothers who had a college/university education and above were included in the study, there was a statistically significant difference between the groups according to the level of parental education. Although the median age of children was significantly higher in the HCWM group (p = 0.005), age groups (< 24 months vs. 24–36 months) and gender distribution was similar in both groups (p = 0.133, p = 0.416).The sociodemographic and parental data of groups are summarized in Table 1.
Changes in the daily routines and family members’ COVID-19 exposure status were presented in Table 2. A significantly higher proportion of mothers in the HCWM group were separated from their children during the pandemic (HCWM vs. non-HCWM: 27.8% vs. 10.8%). Moreover, the duration of separation was significantly longer (20 vs. 3 days, p = 0.002) in the HCWM group. Childcare support by nannies and grandparents and changes in the child’s structured outdoor activities during the pandemic period were more likely observed in the HCWM group (p < 0.05).
BITSEA
Total and subscale scores of the BITSEA, BSI and MSPSS are presented in Fig. 2; Table 1. Although there were no significant differences in children’s BITSEAp median scores between groups, the externalizing and dysregulation scores were significantly higher in the HCWM group (p = 0.031, p = 0.016). There were no significant differences in the BITSEAp and BITSEAc scores between boys and girls (boys vs. girls median BITSEAp 15 vs. 14, p = 0.461; median BITSEAc 17 vs. 17, p = 0.093). The median BITSEAc and total score were significantly higher in the HCWM group (p = 0.030, p = 0.031). Although children above BITSEAp subclinical cut-off were found significantly higher in the HCWM group (30.7% vs. 23.3%, p = 0.044), there was no significant difference between clinical cut-off points. There were no significant differences in mothers’ BSI and MSPSS total and subscale median scores between the groups (Fig. 3; Table 1).
BITSEA, BSI and MSPSS scores for each subscale [* p < 0.05 (Mann-Whitney u test); For each scale first column indicates Group 1 and second column indicates Group 2; BITSEA: brief infant–toddler social and emotional assessment, BITSEAp: The brief infant–toddler social and emotional assessment problem scale, BITSEAc: brief infant–toddler social and emotional assessment competence scale, BSI: Brief Symptom Inventory, MSPSS: Multidimensional Scale of Perceived Social Support]
Distribution of BITSEAp scores above the cut-off [* p < 0.05 at Chi-square test, BITSEAp: The brief infant–toddler social and emotional assessment problem scale, identified cut-offs of BITSEA/P in gender groups for subclinical scores were ≥ 18 for males and ≥ 21 for females. It was ≥ 24 for clinical scores in both genders]
While other BSI subscales and BITSEAp had a mild positive correlation, BSI global index and BITSEAp had a positive moderate correlation (r = 0.412, p < 0.001). All BSI subscales (anxiety, depression, hostility, somatization, negative-self and global index) and BITSEAp subscales (externalizing, internalizing and dysregulation) had a mild positive correlation (p < 0.001). Additionally, the MSPSS total and BSI global index had a negative moderate correlation (r=-0.430, p < 0.001). It was shown that almost all MSPSS and BSI subscales had negative mild to moderate correlations. Bivariate correlation of BITSEA, BSI, MSPSS subscales, sleep parameters and associated sociodemographic variables are summarized in Supplemental File Table 1.
Although there were no significant differences between study groups, it was shown that the percentage of SEB problems in HCWM’s children was significantly higher than national representative data (13.5% vs. 11.9%, with a chi-square test p < 0.001) [28].
In the logistic analysis, male gender (p < 0.001, RR: 3.68, 95% CI: 1.99–6.80), each point increases in BSI global index scores (p < 0.001, RR: 2.56, 95% CI: 1.61–4.09), and having HCWM (p = 0.018, RR: 2.27, 95% CI: 1.15–4.48) were found as the risk factors for BITSEAp scores above the subclinical cut-off. Besides, each point increases in BSI global index scores (p < 0.001, RR: 3.34, 95% CI: 1.91–5.82) was found as a risk factor for clinically significant SEB problems (Table 3).
Sleep
Table 4 provides a summary of maternal perceptions regarding sleep problems and sleep variables based on BISQ. It reveals that both total and night-time sleep durations were significantly shorter in the HCWM group. Furthermore, the HCWM group demonstrated a significantly higher prevalence of perceiving their child’s sleep as a moderate to severe problem.
Changes in sleep patterns and sleep disturbances in children pre- versus post-pandemic were analysed. Changes in sleep pattern were 1.38 times and night wakening’s were 1.8 times higher as compared to the pre-pandemic period in the HCWM group (HCWM vs. non-HCWM group: 41.5% vs. 30% p = 0.004, OR: 1.38; 23.3% vs. 12.9% p = 0.001, OR: 1.80). HCWMs were more likely to perceive their children’s sleep as a moderate to severe problem compared to the non-HCWM group (25.9% vs. 17.1%, p = 0.01, OR: 1.51). Wake-up time was significantly earlier, and night-time and total sleep duration were significantly shorter in the HCWM group (p = 0.004, p = 0.003, p = 0.003). Overall, 22.8% of the study population were classified as poor sleepers and there was no significant difference between the groups (p = 0.097).
Compared with the recent study that represents Türkiye’s nationwide sleep characteristics of the same age group, whole study groups differed significantly from the normative distribution in almost all sleep parameters (Night waking’s increased by 2.63 vs. 2.3, p < 0.001; decreased night-time sleep duration 9.3 vs. 9.6 h, p < 0.001; shorter total sleep duration 11.2 vs. 11.5 h, p = 0.002; increased WASO 59.1 vs. 48.1 min, p = 0.01; decreasing nap number 1.4 vs. 1.6, p < 0.001) [29].
Discussion
There is limited research available on whether children of HCWMs exhibit more SEB problems compared to their peers during the pandemic. Overall, the current study suggests HCWMs have experienced occupational inequality, and young children of HCWMs were at increased risk for externalizing and dysregulation problems during the pandemic. Our findings showed a significantly higher proportion of HCWMs were separated from their children for longer periods. Disrupted childcare support and changes in daily routines have disproportionally impacted HCWMs. Children of HCWMs had higher scores on the externalizing and dysregulation domains of SEB problems than children of non-HCWMs. On the other hand, psychological distress and perceived social support were not different in HCWMs compared to non-HCWMs. Moreover, competence scores were significantly higher in children of HCWMs, suggesting young children of HCWMs may have experienced positive outcomes as well. Maternal psychological distress was found as a potentially modifiable factor affecting the child’s SEB problems. Our findings also showed that these children of HCWMs had higher parent-reported sleep problems, shorter total and night-time sleep, and earlier wake time compared to their peers of non-HCW parents. Moreover, they had an increase in their night wakening and changes in sleep patterns compared to the pre-pandemic period.
Parent-reported SEB problems in infancy and throughout toddlerhood have been reported between 5 and 24% in different studies before the pandemic period [30, 31]. Children of HCWs faced unique stressors, including the risk of their parents contracting the virus, changes in family routines due to their parents’ work schedules, and separation from their parents due to long working hours or quarantine measures. While there is limited research suggesting that children of HCWs may be at increased risk of experiencing SEB problems during the pandemic, the available evidence shows that these stressors can contribute to SEB problems in young children. It is known that externalizing problems are mainly encountered in early childhood because they have limited abilities to communicate about their emotions and use externalizing behaviours to express their emotions [32]. The findings of our study showed young children of HCWMs faced additional stressors such as separation from their parents and disruption of their daily routines due to their parent’s occupations. We also found that children of HCWMs had higher externalizing and dysregulation behaviours compared to their peers. Overall, clinically significant SEB problem was found in 13.5% of the children. The study from Türkiye has shown that parent-reported clinically significant SEB problem was observed in 11.9% of Turkish children aged between 2 and 3 years [28]. In the validation and reliability study of the BITSEA Turkish version, clinically significant SEB problem was found at 13.1% for males and 17.6% for females [23]. In this current study, although there were no significant differences between groups, it was shown that the percentage of SEB problems in HCWM’s children was significantly higher than the nationally representative data [28]. Further, the number of children above BITSEAp subclinical cut-off was found significantly higher in the HCWM group suggesting subclinical difficulties at younger ages may also increase the risk for later psychopathology [32, 33].
Research findings have been mixed and some studies have suggested that children of HCWs may experience positive outcomes as well [34]. Similarly, the current study found that competence scores were significantly higher in children of HCWMs, suggesting young children of HCWMs may have experienced positive outcomes as well. It is important to note that the impact may vary depending on the type of healthcare work their parents are engaged in, the family’s overall social and economic circumstances, and the child’s level of resilience and coping strategies. The current study has not shown a significant difference in perceived social support between HCWMs and non-HCWMs. Social support can take many forms including emotional support, and practical support. It can be particularly important for parents who are experiencing additional challenges. Further research is needed to fully understand the issue.
SEB problems have been linked with high maternal depression and parenting stress [33]. Stress and anxiety levels of parents are associated with children’s SEB [35] and psychological development [36]. During stressful events, children’s emotional adjustment develops and changes mostly depending on the emotional state of their parents [37]. It has been suggested that mothers with depressive symptoms have difficulty responding appropriately in interactions with their children, show less sensitivity to cues from their children, participates less in positive interactions with their children, and cannot use the right strategies to manage their children’s behaviour [38]. Higher total BSI scores of the primary caregiver and being separated from the mother for more than a month were considered clinically significant risk factors for SEB problems in children [39]. Similarly, the study findings showed that higher maternal psychological distress levels were significantly associated with clinically significant SEB problems.
The COVID-19 pandemic has had a significant impact on the daily lives of young children which can contribute to sleep disturbances. In a recent study, it was shown that altered daily routines due to COVID-19 confinement, caused worsened sleep quality in children aged 0–36 months and the caregiver’s stress level was identified as a significant risk factor for this impairment [40]. Similarly, when the parents were asked about the reason for the altered sleep habits, they reported their children slept later than usual, sleep routines were disrupted, did not nap during the day, and had changes in feeding routines [41]. Our study showed that young children of HCWMs faced increased night wakening, earlier wake-up times and shorter night-time and total sleep times than peers. Compared with the recent study that represents Türkiye’s nationwide sleep characteristics of the same age group, almost all the sleep parameters were significantly worse than the normative distribution [29]. Additionally, HCWMs reported that their children’s sleep patterns changed compared to the pre-pandemic period. Sleep problems were found to be associated with SEB problems in the first 3 years of life [42]. Changes in daily routines, and sleep patterns might have contributed to SEB problems in young children who are particularly at a critical stage of social and emotional development. Parents need to establish consistent routines and support healthy sleep habits for young children to address these challenges.
It is important to note that this study only included young children living in Türkiye, and may not be representative of all children of HCWMs. The case-control design of our study did not let us provide information about the causality of SEB and sleep problems. Due to the snowball sampling approach, the generalizability of these findings is limited. To avoid this limitation, we calculated and reached the minimum sampling size to represent our population. The measures used for this study were self-reported. Reliable and valid questionnaires for our country had been used to overcome this limitation. Because the number of children above the clinical cut-off is limited, the significant difference shown in the subclinical cut-off may have not been demonstrated at the clinical cut-off. More research is needed to fully understand the impact of the pandemic on the SEB problems and the well-being of children of HCWMs. The differences between the groups in terms of parental education and family type were notable, although having at least a university/college education was an inclusion criterion. Our aim was to assess mothers’ perceptions but the lack of data on fathers is also a limitation of this study.
The findings of this study suggest that young children of HCWMs were disproportionally affected due to their mothers’ occupations during the COVID-19 pandemic. Addressing psychological distress in HCWMs, improving social support and implementing structured daily routines may serve as potential protective factors for behavioural functioning in these children and thus reduce occupation-related inequalities during the crisis. There is a need for further research into occupational inequality and its potential impact on social and emotional factors particularly for children and parents.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
WHO. COVID-19 weekly epidemiological update, edition 101, 20 July 2022. 2022. World Health Organization. https://iris.who.int/handle/10665/360561.
Gomez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Diaz ZM, Wyssmann BM, et al. COVID-19 in Health-Care workers: a living systematic review and Meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161–75.
Matulevicius SA, Kho KA, Reisch J, Yin H. Academic Medicine Faculty perceptions of work-life balance before and since the COVID-19 pandemic. JAMA Netw Open. 2021;4(6):e2113539.
Diver S, Buccheri N, Ohri C. The value of healthcare worker support strategies to enhance wellbeing and optimise patient care. Future Healthc J. 2021;8(1):e60–6.
Halley MC, Mathews KS, Diamond LC, Linos E, Sarkar U, Mangurian C, et al. The intersection of Work and Home challenges Faced by Physician Mothers during the Coronavirus Disease 2019 pandemic: a mixed-methods analysis. J Womens Health (Larchmt). 2021;30(4):514–24.
Kızılırmak B, Memiş E, Toksöz G. Turkey’s gender equality performance from 2000 to 2019: A rights-based analysis via undp human development and gender development indices. CEİD Association for Gender Equality & UNDP Turkey. 2022:1–92. https://dspace.ceid.org.tr/xmlui/handle/1/2035.
Skokauskas N, Leventhal B, Cardeli EL, Belfer M, Kaasboll J, Cohen J. Supporting children of healthcare workers during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2022;31(1):203–4.
Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378(9799):1325–38.
Moran G, Forbes L, Evans E, Tarabulsy GM, Madigan S. Both maternal sensitivity and atypical maternal behavior independently predict attachment security and disorganization in adolescent mother-infant relationships. Infant Behav Dev. 2008;31(2):321–5.
Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. 2020;75(5):631–43.
Zhang J, Deng X, Liu H, Xu X, Fang R. Evaluation of the mental health status of community healthcare workers during the COVID-19 outbreak. Med (Baltim). 2021;100(6):e24739.
Çiçek S, Yalçin SS. Emotional status and problem behavior of pre-school children according to the pandemic period and occupational status of the mother. Int J Environ Health Res. 2023;33(12):1406–1417. https://doi.org/10.1080/09603123.2022.2096208.
Altinel Açoğlu E, Aydin B, Isiyel E, Çelik M, Yalçın SS. Mother’s psychopathological conditions and parenting characteristics according to smoke exposure. Int J Environ Health Res. 2024;34(3):1701–1712. https://doi.org/10.1080/09603123.2023.2234844.
Yildiz D, Yalcin SS. Change in screen time of preschool children according to parental attitudes during the COVID-19 pandemic with an online survey. Int J Environ Health Res. 2024;34(2):864–873. https://doi.org/10.1080/09603123.2023.2179027.
Boran P. Bebeklik dönemi uyku sorunları ve çözümleri. Yalçın SS, editör. İlk İki Yaşta Sık Karşılaşılan Sorunlar. 1. Baskı. Ankara: Türkiye Klinikleri Pediatrik Bilimler-Özel Konular. 2018;14(4):403–10.
Boran P. Çocuklarda normal uyku fizyolojisi ve farklı gelişim dönemlerinde uyku sorunları. İlk Beş Yaşta Çocuk Sağlığı İzlemi. 2017:331 – 43.
Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics. 2004;113(6):e570–7.
Boran P, Ay P, Akbarzade A, Küçük S, Ersu R. Translation into Turkish of the expanded version of the Brief Infant Sleep Questionnaire and its application to infants. Marmara Medical Journal 2014;27:178–183.
Teng A, Bartle A, Sadeh A, Mindell J. Infant and toddler sleep in Australia and New Zealand. J Paediatr Child Health. 2012;48(3):268–73.
Henderson JM, France KG, Blampied NM. The consolidation of infants’ nocturnal sleep across the first year of life. Sleep Med Rev Aug. 2011;15(4):211–20.
Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The brief infant-toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol. 2004;29(2):143–55.
Alakortes J, Fyrsten J, Carter AS, Moilanen IK, Ebeling HE. Finnish mothers’ and fathers’ reports of their boys and girls by using the brief infant-toddler Social and Emotional Assessment (BITSEA). Infant Behav Dev. 2015;39:136–47.
Karabekiroglu K, Rodopman-Arman A, Ay P, Ozkesen M, Akbas S, Tasdemir GN, et al. The reliability and validity of the Turkish version of the brief infant-toddler social emotional assessment (BITSEA). Infant Behav Dev. 2009;32(3):291–7.
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41.
Eker D, Arkar H, Yaldız H. Çok Boyutlu Algılanan Sosyal Destek Ölçeği’nin gözden geçirilmiş formunun faktör yapısı, geçerlik ve güvenirliği. Türk Psikiyatri Dergisi. 2001;12(1):17–25.
Derogatis L. Brief Symptom Inventory (Baltimore, Clinical Psychometric Research). Psychopathology. 1975;27(1–2):14–8.
Sahin NH, Durak A. Kisa Semptom Envanteri (brief Symptom Invetory-BSI): Turk Gencleri Icin Uyarlanmasi. Türk Psikoloji Dergisi; 1994.
Erol N, Simsek Z, Oner O, Munir K. Behavioral and emotional problems among Turkish children at ages 2 to 3 years. J Am Acad Child Adolesc Psychiatry. 2005;44(1):80–7.
Boran P, Ergin A, Us MC, Dinleyici M, Velipasaoglu S, Yalcin SS, et al. Young children’s sleep patterns and problems in paediatric primary healthcare settings: a multicentre cross-sectional study from a nationally representative sample. J Sleep Res. 2022;31(6):e13684.
Baillargeon RH, Sward GD, Keenan K, Cao G. Opposition-defiance in the Second Year of Life: a Population-based Cohort Study. Infancy. 2011;16(4):418–34.
Moricke E, Lappenschaar GA, Swinkels SH, Rommelse NN, Buitelaar JK. Latent class analysis reveals five homogeneous behavioural and developmental profiles in a large Dutch population sample of infants aged 14–15 months. Eur Child Adolesc Psychiatry. 2013;22(2):103–15.
Gardner F, Shaw DS. Behavioral problems of infancy and preschool children (0–5). In Rutter M, Bishop D, Pine D, Scott S, Stevenson J, Taylor E, Thapar A (Eds.), Rutter’s child and adolescent psychiatry. 5th ed. Wiley Blackwell. 2008;882–893. https://doi.org/10.1002/9781444300895.ch53.
Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are infant-toddler social-emotional and behavioral problems transient? J Am Acad Child Adolesc Psychiatry. 2006;45(7):849–58.
Karaaslan BT, Akoğlu G, Özyurt G, Oral E. Changes in emotion regulation skills of school age children from the eyes of healthcare workers during the COVID-19 pandemic in Turkey: a cross-sectional study. Health Sci Rep. 2023;6(1):e964.
Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, et al. A Meta-analysis of maternal prenatal depression and anxiety on child Socioemotional Development. J Am Acad Child Adolesc Psychiatry. 2018;57(9):645–57. e8.
Verkuijl NE, Richter L, Norris SA, Stein A, Avan B, Ramchandani PG. Postnatal depressive symptoms and child psychological development at 10 years: a prospective study of longitudinal data from the South African birth to twenty cohort. Lancet Psychiatry. 2014;1(6):454–60.
Shorer M, Leibovich L. Young children’s emotional stress reactions during the COVID-19 outbreak and their associations with parental emotion regulation and parental playfulness. Early Child Dev Care. 2022;192(6):861–71.
Chung FF, Wan GH, Kuo SC, Lin KC, Liu HE. Mother-infant interaction quality and sense of parenting competence at six months postpartum for first-time mothers in Taiwan: a multiple time series design. BMC Pregnancy Childbirth. 2018;18(1):365.
Karabekiroglu K, Uslu R, Kapci-Seyitoglu EG, Ozbaran B, Oztop DB, Ozel-Ozcan O, et al. A nationwide study of social-emotional problems in young children in Turkey. Infant Behav Dev. 2013;36(1):162–70.
Markovic A, Muhlematter C, Beaugrand M, Camos V, Kurth S. Severe effects of the COVID-19 confinement on young children’s sleep: a longitudinal study identifying risk and protective factors. J Sleep Res. 2021;30(5):e13314.
Wearick-Silva LE, Richter SA, Viola TW, Nunes ML, Group C-SR. Sleep quality among parents and their children during COVID-19 pandemic. J Pediatr (Rio J). 2022;98(3):248–55.
Makela TE, Kylliainen A, Saarenpaa-Heikkila O, Paavonen EJ, Paunio T, Leppanen JM et al. Signaled night awakening and its association with social information processing and socio-emotional development across the first two years. Sleep. 2021;44(12).
Acknowledgements
We would like to thank the children and their families who participated in this study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Mahmut Caner Us, Perran Boran, Sıddika Songül Yalçın. Mahmut Caner Us, Perran Boran, Sıddika Songül Yalçın, Refia Gözdenur Savcı, Bahar Kural collected data. The first draft of the manuscript was written by Mahmut Caner Us, Perran Boran, Songül Yalçın, Bahar Kural, Dilşad Foto Özdemir and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest disclosure
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Marmara University Faculty of Medicine Clinical Research Ethics Committee; date of approval: 17/08/2020 and protocol number: 09.2020.942.
Consent to participate
The study participants were only mothers who have a child aged 6 to 36 months. Informed consent via online checking was obtained from all the participating mothers. Subsequently, these mothers can access the Google Survey Form.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Congresses
This paper was presented as oral presentation at the Social Pediatric Society of Turkey’s in the selected abstracts of the 2nd International Eurasian Social Pediatric congress organized in Istanbul (Turkey) between October 26th-29th 2022. “SS-66”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Bivariate correlation of variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Us, M.C., Boran, P., Yalçın, S.S. et al. Social-emotional and behavioural problems in young children of healthcare worker mothers during the COVID-19 outbreak: a case-control study. BMC Psychiatry 24, 407 (2024). https://doi.org/10.1186/s12888-024-05801-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05801-4