- Research article
- Open access
- Published:
Fetal alcohol spectrum disorder: neurodevelopmentally and behaviorally indistinguishable from other neurodevelopmental disorders
BMC Psychiatry volume 19, Article number: 322 (2019)
Abstract
Background
The lack of universally accepted diagnostic criteria and the high rate of psychiatric comorbidity make it difficult to diagnose Fetal Alcohol Spectrum Disorder (FASD). In an effort to improve the diagnosis of FASD, the current study aimed to identify a neurodevelopmental profile that is both sensitive and specific to FASD.
Methods
A secondary analysis was conducted on data obtained from the Canadian component of the World Health Organization International Study on the Prevalence of FASD. Data on neurodevelopmental status and behavior were derived from a battery of standardized tests and the Child Behavior Checklist for 21 children with FASD, 28 children with other neurodevelopmental disorders, and 37 typically developing control children, aged 7 to 11 years. Two latent profile analyses were performed to derive discriminative profiles: i) children with FASD compared with typically developing control children, and ii) children with FASD compared with typically developing control children and children with other neurodevelopmental disorders. The classification function of the resulting profiles was evaluated using the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Confidence intervals (CIs) were approximated using 10,000 bootstrapped samples.
Results
The neurodevelopmental profile of FASD tested consisted of impairments in perceptual reasoning, verbal comprehension, visual-motor speed and motor coordination, processing speed (nonverbal information), attention and executive function, visuospatial processing, and language, in combination with rule-breaking behavior and attention problems. When children with FASD were compared with typically developing control children, a 2-class model fit the data best and resulted in a sensitivity of 95.2% (95% CI: 84.2–100.0%), specificity of 89.2% (95% CI: 78.4–97.5%), PPV of 83.3% (95% CI: 66.7–96.2%), and NPV of 97.1% (95% CI: 90.3–100.0%). When children with FASD were compared with typically developing control children and children with other neurodevelopmental disorders, the neurodevelopmental profile correctly identified only 56.9% (95% CI: 45.1–69.2%) of typically developing children and children with other neurodevelopmental disorders as not having FASD, and thus the profile was found not to be specific to children with FASD.
Conclusion
The findings question the uniqueness of children with FASD with respect to their neurodevelopmental impairments and behavioral manifestations.
Background
Exposure to alcohol prenatally is the etiological cause of Fetal Alcohol Spectrum Disorder (FASD) – a term that is used to cover a range of diagnoses, including: Fetal Alcohol Syndrome (FAS), Partial FAS (pFAS), Alcohol-Related Neurodevelopmental Disorder (ARND), and depending on the diagnostic guideline, Alcohol-Related Birth Defects [1, 2]. Although historically used as a non-diagnostic umbrella term, it has recently been proposed that FASD be used as a diagnostic term with the specification of the presence or absence of sentinel facial features [3]. This is in agreement with the newly proposed diagnosis of Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [4]. ND-PAE encompasses a range of neurobehavioral effects associated with prenatal alcohol exposure, and can be diagnosed independent of any physical findings [5].
It is well documented that individuals with FASD exhibit a broad array of neurodevelopmental impairments, such as deficits in adaptive function, attention, executive function, motor function, social cognition, verbal and nonverbal learning, as well as externalizing behaviors [6, 7]. It is also commonly reported that children with FASD have diminished intellectual functioning [8]; however, when compared with IQ-matched control children, differences in their neurodevelopmental presentation have been noted [9]. Although it is widely accepted that the neurodevelopmental and behavioral effects of prenatal alcohol exposure are far-reaching [7], the current diagnostic guidelines tend to focus on the severity of the neurodevelopmental impairments rather than on the specific impairments.
Early and accurate diagnosis of FASD is crucial to providing timely developmental interventions, which are key to altering the developmental trajectory of affected individuals with respect to social functioning, improving their quality of life, and preventing subsequent adverse outcomes common among individuals with FASD, such as school failure and dropping out, addiction, mental health problems, dependent living, as well as involvement with the law and incarceration [10]. However, even in clinical settings where FASD is an important area of emphasis, individuals who have been affected by prenatal alcohol exposure often go undiagnosed or are misdiagnosed [11]. This can likely be attributed to the fact that the diagnosis of FASD is complicated due to difficulties in obtaining confirmation of prenatal alcohol exposure, a high rate of psychiatric comorbidity [12, 13], and the existence of signs and symptoms that overlap with those of other neurodevelopmental disorders [14].
Thus, with the aim of improving screening and diagnostic efforts, the concept of a unique neurodevelopmental profile of FASD, defined as the outward expression (behavioral and developmental) of the central nervous system damage caused by prenatal alcohol exposure, has received some attention in recent years. A distinct neurodevelopmental profile of FASD could assist in accurately identifying individuals with FASD, distinguishing between FASD and other conditions that present similar clinical features, improving clinical services for individuals with FASD, and triaging of individuals most in need of a full multidisciplinary FASD diagnostic assessment. Further, a unique neurodevelopmental profile of FASD could aid in the ascertainment of accurate prevalence estimates, as well as the planning and development of appropriate targeted interventions for individuals with FASD. Therefore, the objective of the current study was to identify a neurodevelopmental profile that is both sensitive and specific to FASD.
As discussed above, FASD includes several distinct diagnoses. As such, there is the possibility that individuals with FASD exhibit more than one neurodevelopmental profile (i.e., a unique profile could exist for each diagnostic category). In order to explore this possibility, the current study utilized a methodology that allows for the empirical determination of the number of distinct profiles.
Methods
Participants
This study was a secondary analysis of data for 37 typically developing children (70.3% male; mean [standard deviation (SD)] age: 9.0 [1.0] years), 21 children with FASD (52.4% male; mean [SD] age: 9.7 [0.8] years), and 28 children with other neurodevelopmental disorders (Attention Deficit Hyperactivity Disorder [ADHD] and/or Autism Spectrum Disorder [ASD]; 75.0% male; mean [SD] age: 9.3 [1.0] years) from the Canadian component of the World Health Organization (WHO) International Study on the Prevalence of FASD [15]. The Canadian FASD prevalence study employed a cross-sectional, observational design using active case ascertainment, along with retrospective collection of prenatal alcohol exposure information, to identify cases of suspected FASD among elementary school students in grades 2, 3, and 4 attending public school in the Greater Toronto Area in Ontario, Canada. The study procedures followed a step-wise approach, where only those students meeting predetermined criteria proceeded to the subsequent phase. Phase I involved: 1) taking growth measurements, 2) identifying learning and/or behavioral problems, and 3) a dysmorphology examination. Phase II involved: 1) a neurodevelopmental assessment, 2) maternal interview, and 3) behavioral observations/ratings by parents, obtained via the Child Behavior Checklist (CBCL) [15]. In addition, a group of typically developing control children was randomly selected from a list of all students who completed Phase I and who did not meet the criteria for Phase II using a systematic sampling technique; these students underwent a complete assessment in Phase II. Final diagnostic screening conclusions were made, by consensus, by a team of experienced multidisciplinary experts, using the 2005 Canadian diagnostic guidelines [1]. A detailed description of the methodology of the Canadian FASD prevalence study is presented in Popova et al. [16].
Measures
Neurodevelopmental assessment
Neurodevelopmental assessments were conducted by qualified psychometrists using the WHO International Study on the Prevalence of FASD test battery, which included: Wechsler Abbreviated Scales of Intelligence, Second Edition (WASI-II [17]; subtests administered included block design, matrix reasoning, similarities, and vocabulary); Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV [18]; subtests administered included coding, digit span, symbol search, and letter-number sequencing); and NEPSY, Second Edition (NEPSY-II [19]; subtests administered included arrows, auditory attention, fingertip tapping, response set, and word generation). This test battery was devised based on the minimum measurements necessary to screen children for FASD, as per expert opinion. All tests were administered and scored by the examiner according to published test manuals and rechecked by a second examiner. Raw scores were converted to scaled scores according to age and sex norms. Canadian norms were used for the WISC-IV, and US norms were used for the WASI-II and NEPSY-II (as Canadian norms are not available for the respective instruments).
Behavioral observations/ratings by parents
Parents were asked to complete the CBCL to evaluate their child’s social competencies and identify any behavioral problems. The CBCL is a widely used, standardized questionnaire to assess emotional and behavioral problems in children aged 6–18 years [15]. T-scores were computed for 23 composite scales using 113 behavioral descriptors, scored on a three-point Likert scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true), according to age and sex norms.
Latent profile analysis
Analysis 1: children with FASD vs. typically developing control children
Latent profile analysis (LPA) [20] was first performed on a sample of children with FASD and typically developing control children in order to identify the measures that best differentiate the two groups of participants. A step-wise approach was used to select indicator variables for the LPA. A total of 42 variables were available for consideration (22 derived from the subtests of the neurodevelopmental test battery and 20 derived from the composite scales of the CBCL). Variables were initially selected based on standardized differences in means between children with FASD and typically developing control children (measured through Cohen’s d) [21]; variables with a large effect size (d ≥ 0.8) were retained. Pearson’s correlation coefficients (r) were calculated to avoid the inclusion of redundant variables. For strongly correlated variables (r ≤ − 0.7 or r ≥ 0.7), the variable with the larger effect size was retained. If the effect sizes were equal, Student’s unpaired t-tests were performed (to test differences in the means between children with FASD and typically developing control children), and the variable with the larger t-score was retained.
Post-hoc analysis
High levels of prenatal alcohol exposure have been found to be associated with an increased risk of impaired intellectual functioning [8]. In order to determine if children with FASD are distinguishable from typically developing control children by IQ alone, LPA was performed using IQ (i.e., the WISC-IV, FSIQ-4 score) only.
Analysis 2: children with FASD vs. typically developing control children and children with other neurodevelopmental disorders
To determine whether the neurodevelopmental profile identified in analysis 1 is specific to FASD, LPA was performed on the complete sample (i.e., children with FASD, children with other neurodevelopmental disorders, and typically developing children). In addition to the class solution selected based on model fit, as described below, a 4-class model was also explored as there were four diagnostically distinct groups included in the sample (FASD, ADHD, ASD, and typically developing children).
Sensitivity analysis
Given the small number of children with ASD in the group of children with other neurodevelopmental disorders and the shared characteristics of FASD and ASD [22], LPA was performed on a sample of children with FASD (n = 21), children with ADHD (n = 22), and typically developing control children (n = 37) to determine the influence that the inclusion of children with ASD had on the ability of the neurodevelopmental profile to differentiate the respective groups of children.
Model selection
The number of subgroups in the sample was tested iteratively based on the following model fit statistics: Akaike Information Criterion (AIC) [23], Bayesian Information Criterion (BIC) [24], log likelihood, and the Lo-Mendell-Rubin adjusted log likelihood ratio test [25]. Optimal model fit was defined by lower relative AIC and BIC values and higher log likelihood values. Further, an entropy value > 0.8 was used as an indicator of highly discriminating latent classes (i.e., an indicator of low classification uncertainty) [26].
Model evaluation
In LPA, following the determination of the likely number of classes, participants were subsequently assigned to a subgroup based on the probability of membership as indicated by the model. This assignment allows for the model’s classification function, as a binary classification test, to be evaluated. This evaluation was achieved through the calculation of the resulting model’s sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). The 95% confidence interval (CI) for each measure of interest was approximated using the 2.5th and 97.5th percentiles of 10,000 bootstrap generated estimates. Further, Cohen’s d and unpaired Student’s t-test for normally distributed data were used to compare the resulting subgroups on each of the observed indicator variables.
Missing data imputation
Little’s missing completely at random (MCAR) test [27] was performed to test the assumption that missing data were missing completely at random (X2(3) = 2.575, p = 0.462); this was confirmed. As such, missing data (0.5% of the data were missing) were replaced by the mean score of the complete cases in the study sample (i.e., mean imputation).
Statistical software
Variable selection and the MCAR test were performed using Stata version 15.1 [28], the LPA was conducted using Mplus version 8.0 [29], and CIs were computed in R version 3.4.4 [30]. Statistical significance was based on an acceptable type-I error rate (α) of 0.05.
Results
The three groups of children differed from one another with respect to ethnicity (p = 0.020), height ≤ 10th percentile (p = 0.041), and occipitofrontal circumference ≤ 10th percentile (p = 0.011). With respect to mean IQ, both children with FASD (mean = 87.2 [SD = 10.2]) and children with other neurodevelopmental disorders (mean = 95.6 [SD = 14.1]) differed from typically developing control children (mean = 106.4 [SD = 12.9]; p = < 0.001 and p = 0.003, respectively), but were not significantly different from one another (p = 0.064). The groups did not significantly differ from one another on age, sex, handedness, weight ≤ 10th percentile, or the three characteristic facial features that discriminate individuals with and without FAS or pFAS (i.e., palpebral fissure length 2 standard deviations below the mean, smooth philtrum, and thin vermillion border). Demographic and descriptive data for study participants are presented in Table 1.
Analysis 1: children with FASD vs. typically developing control children
Based on the variable selection process, described above, ten observed indicator variables were retained. Eight variables were derived from the neurodevelopmental test battery (WASI-II - block design, similarities, and vocabulary; WISC-IV - coding and symbol search; and NEPSY-II - response set, arrows, and word generation (letters)), and two variables were derived from the CBCL (attention problems and rule breaking behavior). Based on the model fit statistics, a 2-class model best fit the data (see Table 2 for the model fit statistics).
In this model, 24 participants (41.4% of the sample) were assigned to subgroup 1, and 34 participants (58.6% of the sample) were assigned to subgroup 2. Participants in subgroup 1 performed worse than participants in subgroup 2 for each of the above eight observed variables derived from the subtests of the neurodevelopmental test battery and scored higher on the above two observed variables derived from the composite scales of the CBCL (Table 3).
The final 2-class model resulted in 91.4% of participants being classified correctly overall, with almost all (20 out of 21; 95.2% [sensitivity], 95% CI: 84.2–100.0%) children with FASD assigned to subgroup 1, and notably more (33 out of 37; 89.2% [specificity], 95% CI: 78.4–97.5%) typically developing control children assigned to subgroup 2 (Table 4).
Post-hoc analysis: latent profile analysis based on IQ only
When IQ was included as the only indicator variable, a 1-class model fit better than a 2-class model (Table 2). As such, the respective model was not explored further. Although the mean IQs for children with FASD and for typically developing control children were found to be significantly different (87.2 [SD = 10.2] vs. 106.4 [SD = 12.9], respectively; p < 0.001), the post-hoc analysis demonstrated that these two groups of children could not be differentiated based on IQ only.
Analysis 2: children with FASD vs. typically developing control children and children with other neurodevelopmental disorders
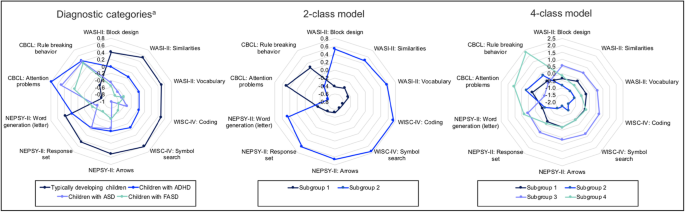
A 2-class model best described the overall sample (Table 2), and correctly identified 83.8% (31 out of 37 [specificity]; 95% CI: 71.0–94.3%) of typically developing children as not having either FASD or other neurodevelopmental disorders (Table 5). However, the 2-class model was only able to correctly identify 56.9% (37 out of 65 [specificity]; 95% CI: 45.1–69.2%) of children with other neurodevelopmental disorders and typically developing children as not having FASD. The 2-class model resulted in almost all children with FASD (20 out of 21) and considerably more children with other neurodevelopmental disorders (22 out of 28) being assigned to subgroup 1, and significantly more typically developing children (31 out of 37) being assigned to subgroup 2 (Table 5). As would be expected, participants in subgroup 1 performed worse than participants in subgroup 2 for each of the eight observed variables derived from the neurodevelopmental subtests and scored higher on the two observed variables derived from the CBCL (Table 3 and Fig. 1).
Mean scores for each diagnostic category and subgroup in the 2- and 4-class models in analysis 2. ADHD: Attention Deficit Hyperactivity Disorder; ASD: Autism Spectrum Disorder; CBCL: Child Behavior Checklist; FASD: Fetal Alcohol Spectrum Disorder; NEPSY-II: NEPSY, Second Edition; WASI-II: Wechsler Abbreviated Scales of Intelligence, Second Edition; WISC-IV: Wechsler Intelligence Scale for Children, Fourth Edition. aChildren with comorbid diagnoses are not included. Note. All scores are presented as z-scores. In the 2-class model, subgroup 1 is comprised of 20 children with FASD, 22 children with other neurodevelopmental disorders, and six typically developing children; and subgroup 2 is comprised of one child with FASD, six children with other neurodevelopmental disorders, and 31 typically developing children. In the 4-class model, subgroup 1 is comprised of 13 children with FASD, 15 children with other neurodevelopmental disorders, and six typically developing children; subgroup 2 is comprised of five children with FASD and four children with other neurodevelopmental disorders; subgroup 3 is comprised of five children with other neurodevelopmental disorders and 31 typically developing children; and subgroup 4 is comprised of three children with FASD and four children with other neurodevelopmental disorders
The 4-class model resulted in all 21 children with FASD and most children with other neurodevelopmental disorders (23 out of 28) being assigned to subgroup 1, 2, or 4, and the majority of typically developing children (31 out of 37) being assigned to subgroup 3. However, the 4-class model did not produce subgroups that were reflective of the diagnostic constructs represented in the sample (see Fig. 1); the model correctly identified only 55.4% (36 out of 65 [specificity]; 95% CI: 43.5–67.2%) of children with other neurodevelopmental disorders and typically developing children as not having FASD.
Sensitivity analysis
A 2-class model best fit the data (Table 2). However, the 2-class model was only able to correctly identify 62.7% (37 out of 59 [specificity]; 95% CI: 50.0–74.6%) of children with ADHD and typically developing children as not having FASD (Table 5). Thus, although children with FASD performed most similarly to children with ASD on the neurodevelopmental subtest included in the profile (Fig. 1), including a small number of children with ASD did not appear to negatively influence the ability of the neurodevelopmental profile to differentiate children with FASD from children with other neurodevelopmental disorders.
Discussion
Although the neurodevelopmental profile identified was sensitive to FASD, it was not specific to FASD, suggesting that a neurodevelopmental profile that can differentiate children with FASD from children with other neurodevelopmental disorders may not exist. However, the findings are limited by the measures used in the analyses, as the inclusion of additional measures may have resulted in a more specific FASD neurodevelopmental profile. Also, data on the use of psychotropic medications were not available. Given that such medications are intended to alter brain function, their use could have impacted the results of the current study. Despite the relatively small sample size, albeit sufficient [31], the latent profile analyses did produce statistically and clinically significant results. Given the few cases of ASD, it was not possible to provide classification results for ASD specifically. Even though the 4-class model did result in children with neurodevelopmental disorders (including FASD) being broken down into subgroups, they were not grouped according to their diagnostic categories. It should be acknowledged that it is possible that the subgroupings could have been an artifact of the methodology used, as the primary goal of LPA is to maximize the homogeneity within subgroups and the heterogeneity between them.
The findings of the current study are in line with those of Mattson and colleagues [32], who were able to demonstrate that a set of neurodevelopmental tests measuring executive function, attention, and visual and spatial memory could differentiate between individuals with FASD and individuals not exposed to alcohol prenatally; however, when using a clinical comparative group, the profile was more accurate at identifying individuals with ADHD than individuals with FASD. Unlike previous studies seeking to identify a unique neurodevelopmental profile of FASD, the current study used a population-based sample of children with FASD – the sample was drawn from a cross-sectional, population-based study that utilized active case ascertainment (the gold standard [33]) to identify cases of FASD. This is also the first study to analyze and incorporate both behavioral observations/ratings of parents and performance-based measures of neurodevelopment when seeking to identify a neurodevelopmental profile of FASD.
Although prenatal alcohol exposure is a necessary cause of FASD, the genetic etiology of FASD remains unknown. Advances in the understanding of genetics and its role in neurodevelopmental disorder risk have created a paradigm shift, such that neurodevelopmental disorders are no longer viewed as having a psychogenic etiology but rather a genetic etiology (see for example, Glessner et al. [34]). Prenatal alcohol exposure leads to epigenetic changes (i.e., altered gene expression) [35]. These changes may contribute to the spectrum of effects and different phenotypes observed in children with FASD [35]. The discovery of reliable genetic and epigenetic markers for FASD would have significant implications for its diagnosis. Such investigations should not be restricted to FASD, but rather include all neurodevelopmental disorders, as this may lead to current categorical classifications of neurodevelopmental disorders being redefined to be more reflective of biologically homogeneous groups [36]. Accordingly, future studies should explore whether neurodevelopmental data combined with genetic and epigenetic data would produce a profile able to diagnose and differentiate FASD from other neurodevelopmental disorders.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADHD:
-
Attention Deficit Hyperactivity Disorder
- AIC:
-
Akaike Information Criterion
- ARND:
-
Alcohol-Related Neurodevelopmental Disorder
- ASD:
-
Autism Spectrum Disorder
- BIC:
-
Bayesian Information Criterion
- CBCL:
-
Child Behavior Checklist
- CI:
-
Confidence interval
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- FAS:
-
Fetal Alcohol Syndrome
- FASD:
-
Fetal Alcohol Spectrum Disorder
- LLV:
-
Log-Likelihood Value
- LPA:
-
Latent profile analysis
- ND-PAE:
-
Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure
- NEPSY-II:
-
NEPSY, Second Edition
- NPV:
-
Negative predictive value
- OFC:
-
Occipitofrontal circumference
- pFAS:
-
Partial Fetal Alcohol Syndrome
- PFL:
-
Palpebral fissure length
- PPV:
-
Positive predictive value
- SD:
-
Standard deviation
- WASI-II:
-
Wechsler Abbreviated Scales of Intelligence, Second Edition
- WISC-IV:
-
Wechsler Intelligence Scale for Children, Fourth Edition
References
Chudley AE, Conry J, Cook JL, Loock C, Rosales T. N. L: Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Can Med Assoc J. 2005;172(5 suppl):S1–S21.
Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais A-S, Manning MA, Robinson LK, Adam MP, Abdul-Rahman O, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256.
Cook JL, Green CR, Lilley CM, Anderson SM, Baldwin ME, Chudley AE, Conry JL, LeBlanc N, Loock CA, Lutke J, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ. 2016;188(3):191–7.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition (DSM-5). Arlington: American Psychiatric Association; 2013.
Kable JA, O'Connor MJ, Olson HC, Paley B, Mattson SN, Anderson SM, Riley EP. Neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE): proposed DSM-5 diagnosis. Child Psychiatry Hum Dev. 2016;47(2):335–46.
Kodituwakku PW. Neurocognitive profile in children with fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15(3):218–24.
Mattson SN, Crocker N, Nguyen TT. Fetal alcohol spectrum disorders: neuropsychological and behavioral features. Neuropsychol Rev. 2011;21(2):81–101.
Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Heavy prenatal alcohol exposure with or without physical features of fetal alcohol syndrome leads to IQ deficits. J Pediatr. 1997;131(5):718–21.
Vaurio L, Riley EP, Mattson SN. Neuropsychological comparison of children with heavy prenatal alcohol exposure and an IQ-matched comparison group. J Int Neuropsychol Soc. 2011;17(3):463–73.
Streissguth A, Barr H, Kogan J, Bookstein FL. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). In: Final report edn. Seattle: University of Washington, School of Medicine; 1996.
Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264–70.
Lange S, Rehm J, Anagnostou E, Popova S. Prevalence of externalizing disorders and autism Spectrum disorders among children with fetal alcohol spectrum disorder: systematic review and meta-analysis. Biochem Cell Biol. 2018;96(2):241–51.
Popova S, Lange S, Shield K, Mihic A, Chudley AE, Mukherjee RAS, Bekmuradov D, Rehm J. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978–87.
McLennan JD. Misattributions and potential consequences: the case of child mental health problems and fetal alcohol spectrum disorders. Can J Psychiatr. 2015;60(12):587–90.
Achenbach T, Rescorla L. Manual for the ASEBA school-age forms and profiles. Burlington: University of Vermont, Research Center for Children Youth & Families; 2001.
Popova S, Lange S, Poznyak V, Chudley A, Shield KD, Reynolds JN, Murray M, Rehm J. Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health. 2019;19(1):845.
Wechsler D. Wechsler abbreviated scale of intelligence–second edition (WASI-II). San Antonio: PsychCorp; 2011.
Wechsler D. Wechsler intelligence scale for children–fourth edition (WISC-IV). San Antonio: PsychCorp; 2008.
Korkman M, Kirk U, Kemp S. NEPSY-II: a developmental neuropsychological assessment. San Antonio: PsychCorp; 2007.
Loehlin JC. Latent variable models, 3rd edition. Mahwah: Lawrence Erlbaum; 1998.
Cohen J. Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale: Lawrence Earlbaum Associates; 1988.
Stevens SA, Nash K, Koren G, Rovet J. Autism characteristics in children with fetal alcohol spectrum disorders. Child Neuropsychol. 2013;19(6):579–87.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–23.
Sclove S. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–43.
Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–78.
Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13:195–212.
Little R. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–202.
Stata Corporation. Statistical software: release 15. College Station: Stata Corporation; 2017.
Muthén L, Muthén B. Mplus user’s guide. 8th ed. Los Angeles: Muthén & Muthén; 2017.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016.
Wurpts IC, Geiser C. Is adding more indicators to a latent class analysis beneficial or detrimental? Results of a Monte-Carlo study. Front Psychol. 2014;5:920.
Mattson SN, Roesch SC, Glass L, Deweese BN, Coles CD, Kable JA, May PA, Kalberg WO, Sowell ER, Adnams CM, et al. Further development of a neurobehavioral profile of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2013;37(3):517–28.
May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome. A summary. Alcohol Res Health. 2001;25(3):159–67.
Glessner JT, Li J, Wang D, March M, Lima L, Desai A, Hadley D, Kao C, Gur RE, Cohen N, et al. Copy number variation meta-analysis reveals a novel duplication at 9p24 associated with multiple neurodevelopmental disorders. Genome Med. 2017;9(1):106.
Liyanage VR, Curtis K, Zachariah RM, Chudley AE, Rastegar M. Overview of the genetic basis and epigenetic mechanisms that contribute to FASD pathobiology. Curr Top Med Chem. 2017;17(7):808–28.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–51.
Acknowledgements
Not applicable.
Funding
No external funding was sought.
Author information
Authors and Affiliations
Contributions
SL led the conception and design of the study, acquired the data, performed the statistical analysis, interpreted the data, and wrote the manuscript; KS contributed to the statistical analysis, data interpretation, and writing of the manuscript; EA contributed to data interpretation and to revising the manuscript; SP and JR contributed to the conception and design of the study, data interpretation, and writing of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was approved by the Research Ethics Board at the Centre for Addiction and Mental Health (Protocol #116/2016).
Consent for publication
Not applicable. The current study utilized secondary, de-identified, anonymized data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lange, S., Shield, K., Rehm, J. et al. Fetal alcohol spectrum disorder: neurodevelopmentally and behaviorally indistinguishable from other neurodevelopmental disorders. BMC Psychiatry 19, 322 (2019). https://doi.org/10.1186/s12888-019-2289-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-019-2289-y